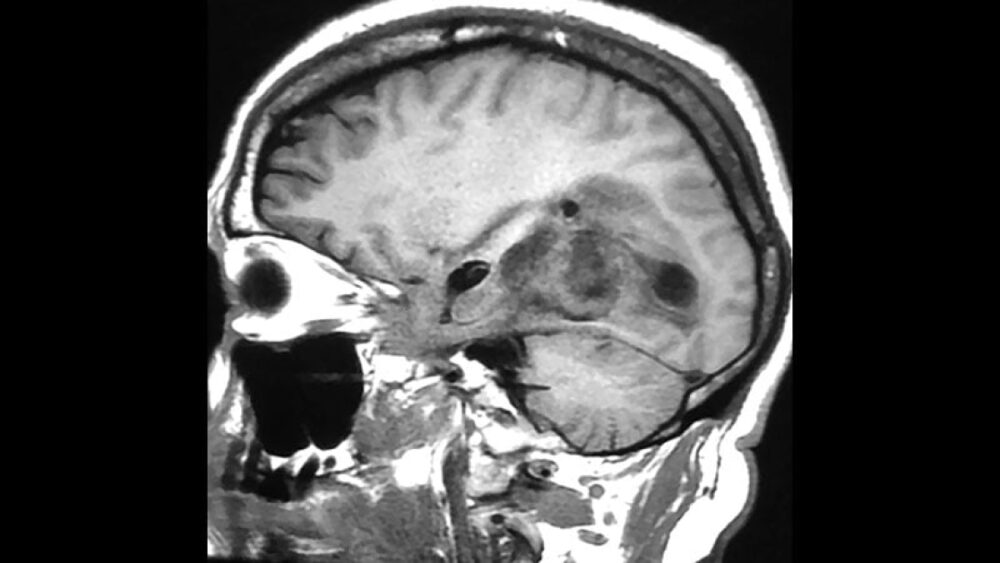
BARCELONA — In a first-in-human clinical trial, an investigational messenger RNA (mRNA)-based cancer vaccine for glioblastoma induced tumor-associated antigen-specific T-cell responses in more than three quarters of patients and had an acceptable safety profile.
“These early data are encouraging,” Ghazaleh Tabatabai, MD, PhD, University Hospital Tübingen, Germany, said in a news release from CureVac, which is developing the vaccine.
“Most importantly, the strong de novo T-cell responses seen in a significant number of patients reflect the vaccine’s ability to break through immune tolerance to the tumor and generate a new immune response,” said Tabatabai, who presented the findings here at the European Society for Medical Oncology (ESMO) 2024 Congress.
MGMT-unmethylated glioblastoma has a poor prognosis, with a median overall survival of roughly 12 months following surgery and chemoradiation with temozolomide. The disease represents a “therapeutic challenge with a high unmet clinical need” for new therapies, Tabatabai told conference attendees.
mRNA vaccines have been shown to induce CD4+ and CD8+ T cell responses against a variety of cancer antigens.
The current investigational multi-antigen mRNA vaccine, CVGBM, encodes eight segments derived from four tumor-associated antigens that are relevant to glioblastoma.
At ESMO, Tabatabai reported the first results from the dose-escalation (part A) portion of a phase 1 study evaluating CVGBM in 16 patients with newly diagnosed and surgically resected MGMT-unmethylated glioblastoma. These patients had also completed post-surgery radiotherapy with or without chemotherapy.
Patients received four dose levels of the vaccine — 12 µg in three patients, 25 µg in three patients, 50 µg in three patients, or 100 µg in seven patients — as seven intramuscular injections within 10 weeks, and optimal maintenance vaccinations at the investigator’s discretion.
Safety and tolerability were the primary outcomes. No dose-limiting toxicities were observed.
Most treatment-related adverse events were grade 1 or 2 systemic reactions characteristic of mRNA-based vaccines. These included headache, chills, fever, and fatigue, which resolved within 1 or 2 days following the injection.
Overall, seven of 16 patients (43.8%) reported a total of nine grade 3 treatment-related adverse events, and no grade 4/5 events. The grade 3 treatment-related adverse events were not dose-dependent. As a result, 100-µg was selected as the recommended dose for the already initiated dose-confirmation (part B) of the study.
Preliminary immunogenicity results showed that the vaccine induced cancer antigen-specific T-cell responses in 10 of 13 evaluable patients (77%), which is “very encouraging,” Tabatabai said.
Most notably, within the group of patients who responded, 84% of immune responses were generated de novo by the CVGBM vaccine, inducing T-cell activity in patients who had no pre-existing T-cell activity against the encoded antigens.
Nine patients (69%) demonstrated antigen-specific CD8+ responses, four (31%) had CD4+ responses, and three (23%) had both a CD8+ and a CD4+ response.
“We are eager to see these results further validated in the next phase of the study,” Tabatabai said in the news release. “This could mark an important moment in the fight against this devastating disease.”
Encouraging Early Data for Other Novel Approaches
The same session featured promising phase 1 results for two other novel therapies to treat brain tumors.
Bart Neyns, MD, PhD, with Vrije Universiteit Brussel, Belgium, reported that intracranial administration of autologous myeloid dendritic cells in combination with ipilimumab and nivolumab in patients with recurrent high-grade glioma was feasible, safe, and associated with “encouraging survival,” warranting further investigation.
Yulun Huang, MD, with the Fourth Affiliated Hospital of Soochow University, Suzhou, China reported that intrathecal injection of allogeneic CAR-γδT cells (QH104) targeting B7H3 for the treatment of recurrent high-grade glioblastoma was safe and led to an objective response rate of 43% and disease control rate of 100%, and a median progression-free survival was not reached after a median follow-up of 7.4 months.
Emeline Tabouret MD, PhD, with University Hospital of Marseille in France, who served as discussant for the three abstracts, agreed that these results are “very encouraging.”
Taking a big-picture view, Tabouret noted that “innovative approaches like mRNA vaccines, dendritic cells, and CAR-T cells are all very promising,” but activity should be improved, and combinations and settings should be better defined.
The study by Tabatabai was funded by CureVac. Tabatabai has disclosed relationships with CureVac and other pharmaceutical companies. The study by Neyns was funded by Kom op tegen Kanker, Belgium. The study by Huang was funded by Unicet Biotech. Neyns, Huang, and Tabouret have reported no relevant financial relationships.